LOS ANGELES ―Treatment drugs can do more than improve the health of people with HIV: If administered early, medications can also reduce the spread of the disease to sexual partners and may help stem the AIDS epidemic.
But many logistical hurdles stand in the way of making this strategy feasible, affordable and effective, according to experts writing in Tuesday’s edition of the journal PLoS Medicine.
The medications in question are antiretroviral therapies, which prevent HIV from multiplying and drastically diminish the amount of virus circulating in the blood. This not only curbs HIV’s assault on the immune system, but it also makes it much more difficult for an infected person to pass the virus to someone else.
This dual benefit was recognized last year in a landmark study finding that people with HIV who received treatment early on, before their immune systems encountered much damage, were 96 percent less likely to transmit the virus to their heterosexual partners than those who received treatment later in the course of the disease, when drug treatment is usually initiated.
One important implication was that HIV treatment and prevention efforts didn’t have to compete for resources, said Dr. Anthony Fauci, director of the National Institute of Allergy and Infectious Diseases, part of the National Institutes of Health. The study prompted AIDS experts to rethink their approach to preventing the virus’ spread. Science magazine named it the “Breakthrough of the Year.”
But capitalizing on this discovery may prove more difficult than some had hoped. Experts are now divided about whether the treatment-as-prevention approach can essentially halt the AIDS epidemic.
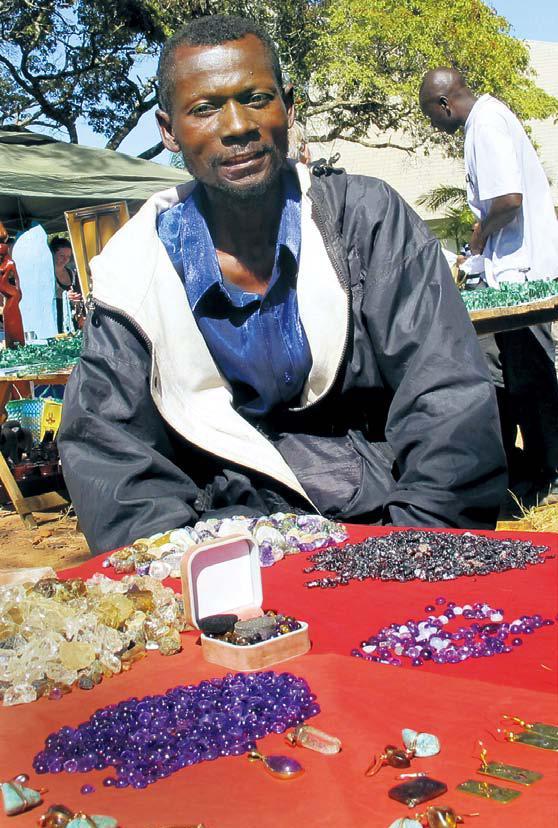
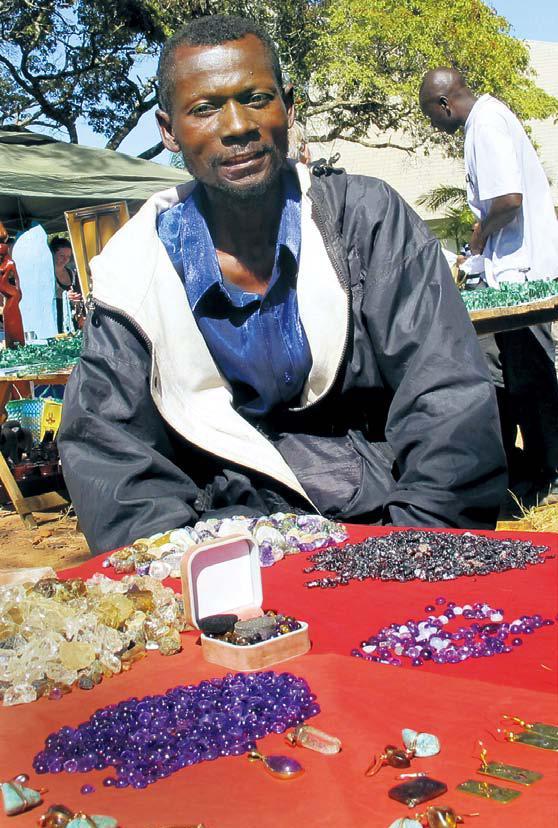 |
Teddy Njapau, a Lusaka jeweler, says U.S.-supplied medications have helped him survive the HIV virus. |
“The field is split about whether it’s really the best thing and it’s going to stop transmission, or if it’s a small part of the puzzle,” said Timothy Hallett, an infectious disease epidemiologist at Imperial College London, who co-wrote one of the new studies.
The real-world experience of public health officials in San Francisco, British Columbia, France and Australia ― four places where HIV testing and drug therapy are already common ― make clear that simply handing out pills won’t be enough to beat back the virus, according to one of the studies.
Australia probably represents a best-case scenario, since antiretroviral drugs are freely available in that country and about 70 percent of people with HIV take the medication. But even there, the number of new HIV diagnoses has increased from 700 per year in 1999 to 1,000 per year in 2011, said study author David Wilson, an epidemiologist at the University of New South Wales in Sydney.
Early treatment “can have an impact, but it’s not going to eradicate HIV,” he said. “It’s not the magic bullet.”
For treatment to double as prevention, people need to get tested for HIV on a regular basis, start antiretroviral treatment once they test positive, and swallow pills for the rest of their lives to manage their viral load. Failure to follow through at any of these stages greatly reduces the drugs’ ability to block transmission, Wilson said.
Making matters worse, people on the medication might stop taking other preventive measures, like using condoms, he added.
Biology and behavior are only two aspects of the treatment-as-prevention strategy that were examined in the PLoS Medicine studies. Some of the papers addressed economic considerations, including how long it would take for expenditures on antiretroviral drugs to pay for themselves by preventing costly treatments in people who remain HIV-free. The answer to that question is important for policymakers who are working with limited budgets.
Study authors also suggested that public health officials prioritize getting drugs to sex workers (who could spread the virus widely if untreated) and pregnant women (to reduce transmission to babies and deaths of mothers), among other groups. However, the authors noted the paucity of data available to evaluate whether these are the right groups to target.
Fauci, who didn’t work on the new studies, said a primary objective is reaching and treating people who don’t know they are infected with HIV, since they unwittingly transmit the majority of new HIV cases each year.
Public health officials in Los Angeles County, which has the country’s second-largest concentration of HIV-positive people, hope to make testing a routine part of health care services to reach such individuals. Mario Perez, director of the county’s HIV and sexually transmitted disease programs, called early treatment a “cornerstone” of the HIV prevention program.
“Getting a much higher proportion of residents living with HIV to be on treatment is going to be crucial to getting ahead of the epidemic,” he said. “If we don’t do that, I think we’re going to continue to limp along with trying to prevent HIV infection.”
And while the costs of drug treatment are much lower than they used to be, thanks in part to the development of generic alternatives to expensive name-brand drugs, other prevention methods like circumcision and condom distribution are far less costly.
Experts stressed that early drug treatment should not be seen as a replacement for other preventive measures.
Though the strategy faces many uncertainties, Fauci said one thing is clear: “Biologically, it absolutely works.” And if it can be successfully implemented, he said, “it would be an absolutely critical part of turning around the trajectory of the AIDS pandemic, in this country and worldwide.”
By Erin Loury
(Los Angeles Times (MCT))
(MCT Information Services)