Scientists reported Wednesday in a provocative new study that they were able to “see” pain on brain scans and, for the first time, measure its intensity and tell whether a drug was relieving it. Though the research is in its early stages, it opens the door to many possibilities.
Scans might be used someday to tell when pain is hurting a baby, someone with dementia or a paralyzed person unable to talk. They might lead to new, less addictive pain medicines. They might even help verify claims for disability.
“Many people suffer from chronic pain, and they’re not always believed. We see this as a way to confirm or corroborate pain if there is a doubt,” said Tor Wager, a neuroscientist at the University of Colorado, Boulder.
He led the research, published in the New England Journal of Medicine. So far it is only on pain felt through the skin ― heat applied to an arm. More study needs to be done on more common kinds of pain, such as headaches, bad backs and pain from disease.
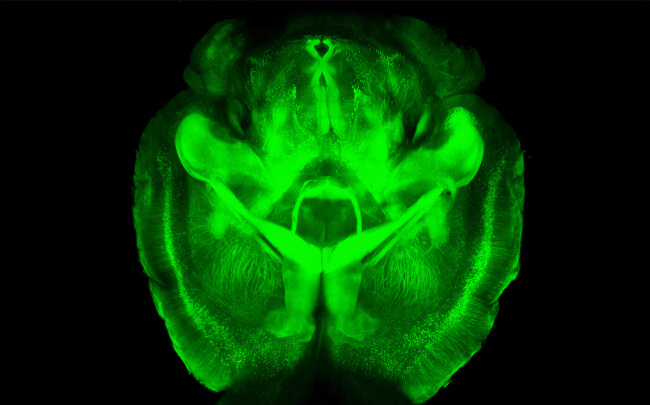 |
This undated image provided by Karl Deisseroth’s lab shows a three-dimensional rendering of clarified mouse brain seen from below. (AP-Yonhap News) |
Pain is the top reason people see a doctor, and there’s no way to quantify how bad it is other than what they say. A big quest in neuroscience is to find tests or scans that can help diagnose ailments with mental and physical components such as pain, depression and PTSD, or post-traumatic stress disorder.
Although many studies have found brain areas that light up when pain is present, the new work is the first to develop a combined signature from all these signals that can be used to measure pain.
“This is very exciting work. They made a huge breakthrough in thinking about brain patterns,” said Dr. David Shurtleff, acting deputy director of the National Institute on Drug Abuse, which helped sponsor the research. “We need a brain-based signature for pain. Self-report doesn’t cut it. It’s not reliable, it’s not accurate.”
The research involved four experiments at Columbia University approved by a panel to ensure no participants were harmed. In all, 114 healthy volunteers were paid $50 to $200 to be tested with a heating element placed against a forearm at various temperatures, not severe enough to cause burns or lasting damage. Some of the experiments required them to stand it for 10 to 20 seconds.
“It’s like holding a hot cup of coffee that you really want to put down but can’t quite yet,” Wager said.
Functional magnetic resonance imaging, or fMRI scans, which don’t require radiation as X-rays do, recorded changes in brain activity as measured by blood flow. Computers were used to generate signatures or patterns from these readings.
The first set of experiments on 20 people developed signatures for pain versus the anticipation of it or mild warmth on the arm. The second experiment validated these signatures in 33 other people and found they predicted how much pain they said they felt.
“It’s really what seems to be a true measure of the experience that the patient’s having,” and it gives a number to pain severity that can guide care, said one expert with no role in the studies, Dr. Costantino Iadecola, director of the Brain and Mind Research Institute at Weill Cornell Medical College.
Researchers took their work a step further with the third experiment, which involved 40 people who recently lost a serious love relationship and were feeling intensely rejected. Besides the heat tests, they had scans while being shown a picture of their former partners and then a picture of a good friend. Researchers found the brain signatures for social or emotional pain were different from the ones for physical pain.
“That’s very provocative,” said Dr. Allan Ropper, a neurologist at Brigham and Women’s and Harvard University who wrote a commentary in the journal. The signatures seem highly accurate and able to distinguish physical pain from other kinds, he said.
In the fourth experiment, researchers gave 21 participants two infusions of a morphine-like drug while they were being scanned and having the heat tests. The first time, they knew they were getting the drug. The second time they were told they were getting dummy infusions but in fact got the drug again. Brain signatures showed their pain was being relieved both times in proportion to how much drug was in their systems.
“This is beginning to open a new wedge into brain science,” Ropper said. “There may be completely novel ways of treating pain by focusing on these areas of the brain rather than on conventional medications which block pain impulses from getting into the spinal cord and brain.”
Shurtleff also said he hoped the research would lead to newer drugs.
“We want medications that can reduce this signature and don’t show a signature for addiction,” he said. (AP)


![[KH Explains] Why Yoon golfing is so controversial](http://res.heraldm.com/phpwas/restmb_idxmake.php?idx=644&simg=/content/image/2024/11/13/20241113050608_0.jpg)




