Upper endoscopy is the most fundamental test to diagnose diseases of the esophagus, stomach and the duodenum (for example, gastric cancer, gastric ulcers, duodenal ulcers and esophagitis). Unlike radiological tests using contrast imaging of the upper gastrointestinal tract, endoscopy allows a direct biopsy of any abnormal tissues, producing a more accurate diagnosis as well as helping the treatment planning. Gastric cancer is very common in Korea and upper endoscopy is very important for early diagnosis of gastric cancer.
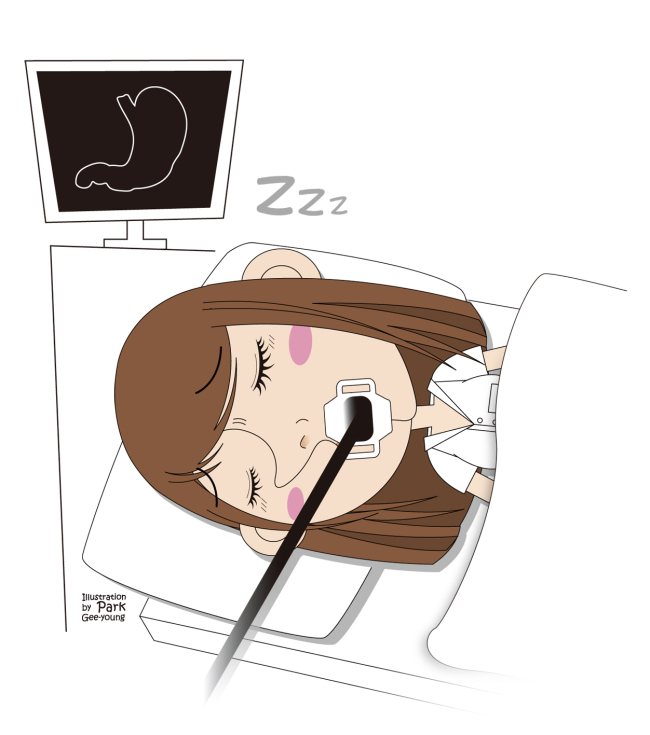 |
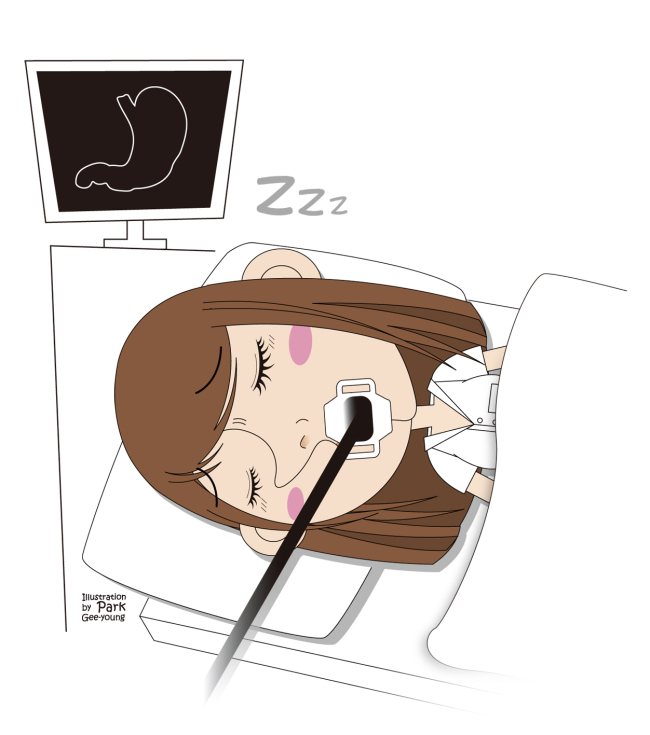
Illustration by Park Gee-young |
Previously, sedation was not used for endoscopies, but more recently, endoscopy under sleep sedation has been used to make the patient more comfortable during the procedure. Unlike the name suggests, the patient is not actually sleeping, but under the effect of sedatives and can respond to the doctor talking to him or her. The patient can also respond to light stimuli during the procedure. Some patients may fall asleep during the procedure, hence the name, but the main purpose of the procedure is not to cause the patient to sleep. The term “conscious sedation” is used more frequently these days. For conscious sedation endoscopy, several medicines are used to sedate the patient to a certain level, to reduce any discomfort during the procedure. However, depending on the patient, some may not reach a sufficient level of sedation, while others may become too sedated, and various complications can occur.
Side effects include respiratory complications such as dyspnea or hypoxia, cardiovascular complications such as tachycardia, and falls, but most patients recover without any treatment. However, in very rare cases, cardio respiratory arrest can occur and pose a fatal risk, and some patients may need emergency treatment due to hypersensitivity reactions. Therefore, special care should be taken in those who have respiratory diseases, lung dysfunction, kidney or heart disease. However, those without previous health problems can still develop serious complications during conscious sedation endoscopy. The patient needs to rest to recover after the procedure, and should not drive on that day. The patient should also avoid important meetings or business for the day.
Several medications can be used for conscious sedation endoscopy. One of the most commonly used agents is midazolam. In Korea, propofol has also been used recently for the said procedure. The advantage of propofol is that it leads to a faster recovery after the procedure than using midazolam. However, it is believed to be associated with a higher risk of developing side effects, such as dyspnea. It is important to monitor the status of the patient during conscious sedation endoscopy and have the appropriate equipment and experienced medical staff to attend to any problems that may arise immediately.
In conclusion, the patient should discuss the procedure fully with medical staff before making the decision to undergo conscious sedation endoscopy. In addition, the medical institute should be sufficiently prepared to monitor the status of the patient and attend to any emergencies that may arise.
By Lee Jun-haeng
The author is a doctor at the Division of Gaestroenterology at Samsung Medical Center and a professor of Sungkyunkwan University School of Medicine. ― Ed.